About Endometrial Cancer
If you or a loved one is living with or at risk for endometrial cancer, it is important to learn all you can about the disease and what to expect. Select a topic below to learn more.
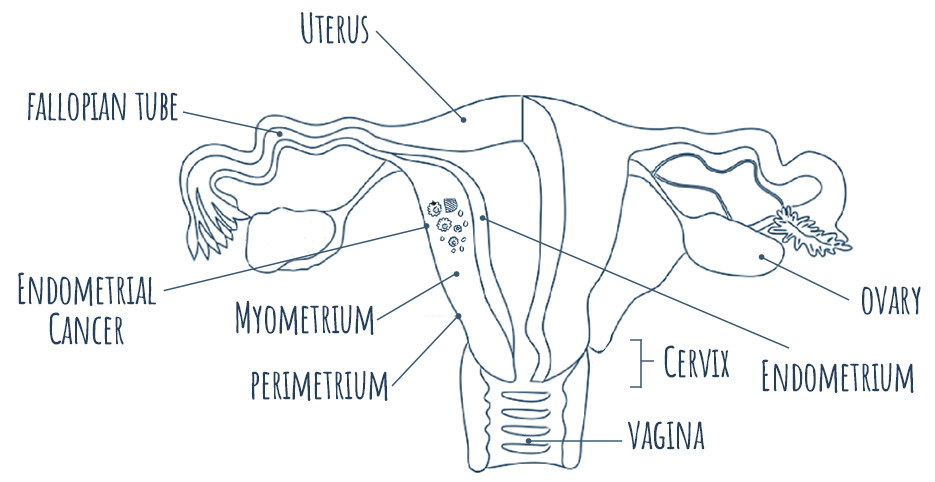
what is Endometrial Cancer?
Endometrial cancer, a type of cancer of the uterus, is found in the inner lining of the uterus, known as the endometrium. It is the most common type of cancer that affects the female reproductive organs.1
Recognizing the Signs and Symptoms of Endometrial Cancer
There are a few signs and symptoms that can point to endometrial cancer. Some become more common as the cancer grows and spreads.2 It’s important to listen to your body and talk to a healthcare provider if you notice any endometrial cancer signs or symptoms. Understanding potential signs and symptoms of endometrial cancer may allow for an earlier diagnosis, when it may be more easily treated.
- Most common sign: Abnormal bleeding from the vagina (bleeding between periods, bleeding after menopause or abnormal vaginal discharge). While non-cancer problems can also cause abnormal bleeding, about 90% of those with endometrial cancer have abnormal bleeding from the vagina.2
- Other signs and symptoms:2
- Non-bloody vaginal discharge
- Pain in the pelvis
- Feeling a mass (tumor) in the pelvic area
- Sudden weight loss
*These are not all the possible signs/symptoms of endometrial cancer, so it is important to talk to your healthcare provider if you notice anything unusual.
Diagnosis
Getting an Endometrial Cancer Diagnosis
Endometrial cancer is most often diagnosed after a person visits their healthcare provider because they are experiencing symptoms.3 There is currently no standard or routine screening test for diagnosing endometrial cancer early in patients who are at average risk and have no symptoms.4 Because of this, it’s important to pay attention to any changes in your body that do not feel normal, and talk to a healthcare professional if you notice anything different. You should also talk to your healthcare provider about when to get pelvic exams, which can find some cancers, including some advanced uterine cancers.5
- Endometrial cancer is usually diagnosed by a few tests after a person experiences symptoms.3
- Pelvic ultrasound (procedure using sound waves to take pictures of the inside of the body)
- Transvaginal ultrasound (in the vagina)
- Endometrial biopsy and tissue sampling
- Additional scans as recommended by your healthcare provider
Endometrial Cancer Staging at Diagnosis
After a patient receives an endometrial cancer diagnosis, the healthcare team determines the stage of the cancer, which describes the amount of cancer in the body, and determines how serious the cancer is and how best to treat it.6
Stages of Endometrial Cancer6
Stage I |
Cancer is found in the uterus only
|
| Stage II | Cancer has spread into the connective tissues of the cervix, but not outside of the uterus |
| Stage III |
Cancer has spread beyond the uterus and cervix, but not beyond the pelvis
|
| Stage IV |
Cancer has spread beyond the pelvis
|
Who Is at risk?
Who is at Increased Risk for Endometrial Cancer?
Several risk factors may increase or decrease the chances of developing endometrial cancer.
Factors that may increase risk7
|
Factors that may reduce risk8
|
How Does Family History Impact my Risk of Endometrial Cancer?
Endometrial cancer can run in families. People with a first-degree family history (mother, sister or daughter) of endometrial cancer have a higher chance of developing the disease than those without.9
Some of these families also have a higher risk for colon cancer – a disorder called hereditary nonpolyposis colon cancer (HNPCC), also known as Lynch Syndrome. People with Lynch Syndrome have up to a 70% chance of developing endometrial cancer – compared to the general risk for women at 3%.7
If you have a family history of endometrial cancer or Lynch Syndrome, you may be at a greater risk for developing the disease. Talk to your healthcare team for more information on understanding your endometrial cancer risk factors.
Tumor Characteristics and testing
Using Endometrial Cancer Biomarkers to Determine Risk and/or Treatment
Biomarkers are specific features in cells, like protein or DNA, that can help determine risk of developing disease and best potential treatment options.3,10 Like many other cancers, endometrial cancer has biomarkers that can be determined through testing.11 Some important biomarkers include:11
-
Estrogen and progesterone receptors (ER/PR) are hormone receptors found in about 60%-75% of endometrial tumors and may help predict positive responses to hormone therapy.12
-
Tumor mutational burden (TMB) measures the number of mutations within a tumor. About 40% of endometrial cancers have high TMB, which is associated with both a better prognosis and better responses to immunotherapy. 13,14,15
-
Polymerase epsilon (POLE) mutations occur in about 10% of endometrial cancers. These patients are less likely to experience the cancer returning or death and also appear to benefit less from chemotherapy and radiation.16
-
Human epidermal growth factor receptor 2 (HER2) proteins are found at high levels in 30% of Stage II endometrial cancers.17 Lower HER2 levels are associated with better survival rates.18
-
Phosphatase and tensin homolog (PTEN) gene mutations occur in about 45% of endometrial cancers.19 PTEN can serve as a warning sign that precancerous tissue is at higher risk of developing into endometrial cancer.20
-
Neurotrophic tyrosine receptor kinase (NTRK) is a relatively rare biomarker among endometrial tumors, but it can be useful for making treatment decisions. For patients who test positive for NTRK, tyrosine kinase (TKI) inhibitors can be used to target cancer cells.21
-
P53 gene mutations occur in about ~25% of patients with endometrial cancer and are generally associated with a poorer prognosis in serous endometrial carcinomas.22
-
Programmed death ligand 1 (PD-L1) is a protein found on the surface of cancer cells in about 34% of patients with endometrial cancer. For these people, treatments targeting PD-L1 may help the immune system find and fight off their cancer.23
-
Mismatch repair deficiency (dMMR), which leads to high microsatellite instability (MSI-H), occurs in about 30% of endometrial cancer patients and is more common in endometrial cancer than other cancer types.24 dMMR/MSI-H have been associated with response to immunotherapy.25
What is Mismatch Repair Deficiency (dMMR)?
-
In normal cells, mismatch repair (MMR) is a process that corrects any errors made when DNA is copied in a cell.26
-
When this repair mechanism doesn’t work correctly, it is known as mismatch repair deficiency (dMMR). dMMR can lead to several DNA errors in a cell, which may lead to cancer.26
-
MMR deficiency contributes to microsatellite instability, which involves many gene mutations.27
-
25 to 35% of patients with endometrial cancer have these mismatch repair deficient (dMMR) tumors.27
of patients with endometrial cancer have these mismatch repair (dMMR) tumors.27
What is Microsatellite Instability (MSI)?
-
Microsatellites are repeating stretches of DNA in your cells. Sometimes microsatellites lead to errors in the DNA-repairing process inside your cells. Typically, these errors are easily fixed by built-in repair processes, like mismatch repair (MMR).28
-
If the repair process does not work, like with MMR, the errors within the microsatellite segments may keep multiplying or increasing, which is known as microsatellite instability.28
-
Understanding if your tumor has high microsatellite instability (MSI-H) may help determine treatments you are eligible for.28
Determining MMR / MSI Status
Immunohistochemistry (IHC)
-
IHC is a testing method to determine MMR status.29
-
IHC is completed in a lab that tests by adding a dye to a tissue sample.30
-
Once the dye is added to the sample, the lab technician takes a closer look through a microscope to determine biomarker status.30
Polymerase Chain Reaction (PCR)
-
Like IHC, PCR is completed in a lab to measure MSI by quickly making millions to billions of copies of a piece of DNA, so that it can be studied more closely.31
Next Generation Sequencing (NGS)
-
NGS is testing also done in a lab, looking at DNA and RNA fragments like they are building blocks. This kind of test puts together the fragments to identify any changes in certain areas as they are placed together.32
-
Healthcare providers can then choose medications that target these genetic changes in the tumor.32
Knowing your biomarker status can help find the treatment option that may be best for you.
Endometrial Cancer Treatment
Endometrial Cancer Treatment Options
Treatment plans for people with endometrial cancer can depend on the stage at which their cancer is diagnosed. It’s important to work with your healthcare team to develop the appropriate treatment plan.33
|
1. Surgery33 Surgery is the most common treatment for endometrial cancer, when possible. It may include:
2. Radiation Therapy33 After the visible cancer cells are removed, some patients may be given radiation therapy that uses high-energy x-rays or other types of radiation to destroy cancer cells or keep them from growing. 3. Chemotherapy33 Your healthcare provider may also consider chemotherapy after your diagnosis. Chemotherapy is a treatment for endometrial cancer that uses medication to stop the growth of cancer cells, either by destroying them or keeping them from dividing. 4. Hormone Therapy33 Another option to treat endometrial cancer is hormone therapy, removing or blocking hormones that can cause certain cancers to grow. 5. Targeted Therapy33 Targeted therapy for endometrial cancer uses medication to identify and attack specific cancer cells. 6. Immunotherapy34 Immunotherapy helps a person’s own immune system better recognize and kill cancer cells. The immune system normally can keep itself from attacking the body’s healthy cells. It does so by using “checkpoint” proteins on immune cells, that act like switches that need to be turned on (or off) to start an immune response. Cancer cells turn these checkpoint proteins “off” to avoid getting attacked by the immune system. Immunotherapies can be used to treat some endometrial cancers by switching the immune response back “on.” |
Endometrial Cancer Recurrence
For many people with endometrial cancer, treatment may remove or destroy the cancer.35 However, there is a possibility that it can come back, or recur, after it’s been treated.33 It may come back in the uterus, pelvis, lymph nodes, or other parts of the body.33
About 13% of endometrial cancers recur,36 the majority of them during the first two years after treatment.37
The possibility of recurrent endometrial cancer can be scary. Patients may feel anxious or uncertain about what to do next, even if their cancer is currently in remission. Understanding what endometrial cancer recurrence means is an important step in choosing the right treatment plan with your healthcare provider and managing the emotions that come along with it.
